My doctor beamed at me. “I feel like if we keep you in, we’ll discover something new about your body every week!”
but we’ll get there…
Happy holidays everyone!
Believe it or not, I’m finally home. I didn’t quite take up residence on node 3, floor 6 south of the Pacific Campus of CPMC, though there were times it may have looked that way.
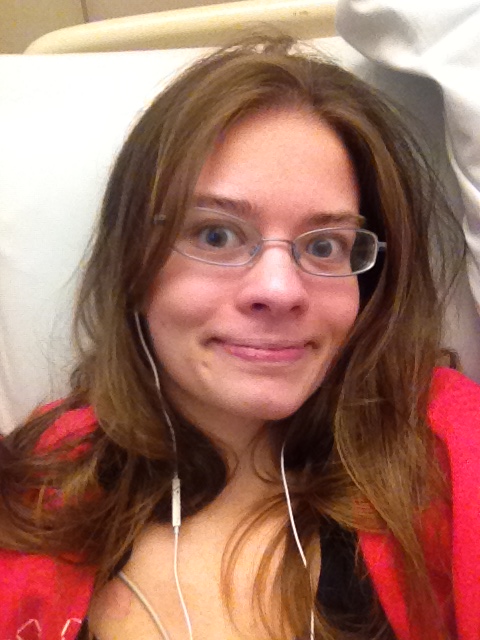
Staying in the hospital for a relatively long time can be uncomfortable and exhausting. There’s no place like home, and the Ozian adage applies when you’re sick too. Even for someone capable of generally sleeping through noise, like I am (particularly notable feats include sleeping through my friends partying in a hotel room with music and a hospital blood draw), the hospital can make it difficult to get a full night’s sleep. While I am technically capable of sleeping through vitals checks and blood draws (especially through my handy PICC line, where I don’t even need to get poked), it becomes a much more difficult pursuit when the nurses and aides have to turn on the light, re-position me to get the correct arm (blood had to be drawn through the PICC arm and blood pressure couldn’t be taken on the PICC arm), take my vitals three times to make sure they’re really that low, etc. It could also be difficult to return to sleep after the early morning check up, including vitals and blood draws, as it would be just close enough (4:30-5:30 usually) to when I would wake up naturally to cause problems. Add in the occasional early morning admission or inconsiderate roommate (4 a. m. is not the time to watch TV on full blast or call everyone in your address book to complain about your bowels!) and sleep could feel elusive. On top of that, I was often in need of more sleep than usual because I was exhausted from various procedures and just from being sick. I did take naps, but there’s nothing like my own bed for a good night’s rest.
And then there’s claustrophobia. I spent almost all of the fifteen days on the sixth floor, with a few sojourns to GI Lab (fifth floor) and radiology/nuclear medicine (second floor.) I didn’t step foot outside the entire time. Believe me when I say that the walk from the hospital entrance to the curb where my dad had the car felt fantastic. Fresh air truly is a wonderful thing. Being cooped up like that could make you go a little bit crazy.
It was also hard being 3.5 hours from home. My parents had to stay in a hotel and we hadn’t realized how long the stay would end up being. You don’t quite have your regular support network when you’re that far from home. (Though I fully acknowledge that I am incredibly lucky to have such a good motility center only a few hours from home! I’ve gotten to know a number of people who have to travel across states or even oceans in order to get the appropriate medical care for their condition!)

There are always the views…and there were far better ones when I went on my blood clot preventing walks around the floor!
All of the inconveniences of the hospital stay pale in comparison to what I got out of it, though.
When I left off in my last post, I think I’d just had my gastric emptying study. I didn’t know my exact emptying time, but I knew that it had looked and felt pretty delayed. On Monday I received news of the precise time: 54% of my simple meal remained in my stomach after four hours. Normal is considered to be under 10%. This kind of delay is indicative of pretty considerable gastroparesis.
Radioactive eggs actually become yummy when you haven’t had anything to eat by mouth in weeks. Yes, I enjoyed eating the meal for the emptying study…at least until the pain and reflux started!
Saturday morning, I wrote an update here, but I don’t think I said much about my cardiac issues other than to mention that my heart rate was having problems. Well, first of all, the good news: my QT interval reverts to normal when I have a good electrolyte balance and avoid even the most mildly prolonging of medications. If I take even “less prolonging” medications, my QTc (corrected interval that accounts for heart rate) gets out of whack. Basically, this means I have to be very careful about what medications I take and there are pretty much no anti-emetics (drugs for nausea) or pro-kinetics (drugs that improve motility) that I can take. That’s less of a sacrifice than it might be because none of the anti-emetics really work on me, unless I get enough of a combination that they just put me to sleep. I talked about this with a couple of my doctors and it’s because my vomiting really isn’t nausea-mediated. For a lot of people, the loop goes nausea -> vomiting -> nausea but for me it’s vomiting -> nausea -> vomiting. If I take drugs that remove nausea from the equation, I may temporarily feel more comfortable, even falsely optimistic, but that soon goes away when I begin vomiting again. I also don’t always have nausea even when I am vomiting. Weird, I know, but it helps explain the lack of efficacy!
More of an ongoing dilemma has been my heart rate. I was put on telemetry (heart monitoring) and a beta blocker because of my long QT at the beginning of the first week. While on the monitor, everyone began to notice that my heart rate would spike considerably at different points through the day. Several times when I got up to go to the bathroom, for example, nurses would race in to ask what was wrong and then tell me my heart rate had gone up. “Oh,” I would say, “I guess it feels a little fast.” I figured it was going up by ten, maybe twenty at most, since I didn’t even feel lightheaded, didn’t see black, didn’t collapse — all things I’ve done in the past with orthostatic intolerance.
My heart rate was reaching into the 160s and 170s when I stood up. Even with the beta blocker.
At about 3 a. m. Saturday morning, a nurse woke me up, with some difficulty. She (or he? my exact memories of that time are a bit blurry) explained that she had to take my blood pressure again. It was 75/33. She said that that was the third time it was in that range and she called the night hospitalist. He came in and talked to me for a minute before looking at my file and putting in a few orders: a pill to bring up my blood pressure, extra fluids, blood cultures to check for a line infection, an IV broad spectrum antibiotic, and discontinuation of the beta blockers until the cardiologist could review my case. (As an aside, the tiny pill I swallowed to bring up my blood pressure is the last thing I kept down.) Don’t worry — I wasn’t septic and I didn’t have an infection. But I wasn’t able to ever really get my blood pressure up high enough to take the beta blocker again. (It’s very normal for me, when relaxed, to run around 100/60, and when I didn’t get massive amounts of saline I was often in the 90s, so I didn’t have all that much room to spare!)
I’ve talked to no fewer than four cardiologists since that point, and everyone agrees that as long as I’m mostly asymptomatic with my tachycardia, no more beta blockers and lots of fluids. My heart rate continued to spike into the 160s or so when I stood and continue around the 140s when I stayed standing up. My resting heart rate was typically in the 80s or so during the day, often dipping into the 50s at night, so I had a lot of variation. Some of this may just be deconditioning, so everyone has encouraged me to keep standing/walking in the hope that will help with this in the future. (When I first went on telemetry, concerned nurses originally made me stay in bed. This meant I got heparin shots to prevent blood clots. I’d rather walk, for a lot of different reasons.) The electrophysiologist I saw in the hospital told me that it’s common to have issues with regulation of heart rate and blood pressure if you also have gastroparesis/motility issues because they all involve the autonomic nervous system. The only weird thing is that I’m asymptomatic, but I’ll take that kind of weirdness! So, for now, I just have postural tachycardia, rather than Postural Orthostatic Tachycardia Syndrome.
My cardiology fellow brought me this guy. She was amazing, both as a doctor and a person, and felt badly about my being inpatient over the holidays. Isn’t he the cutest?!
Back to the star of this show: my stomach! On Monday, I had yet another EGD (upper endoscopy), this time with a pyloric manometry. The pylorus is the valve that separates the stomach from the small bowel and allows the passage of food. Some people with gastroparesis have a pyloric spasm that contributes to their delay in emptying food from their stomachs. For those people, injecting Botox into the pylorus can help. When I went in for the procedure, my doctor said that she would inject Botox if my pylorus had that kind of problem. It turned out that it didn’t, so that ruled that option out.
Also on Monday, I received a diagnosis of idiopathic gastroparesis. While some gastroparesis stems from diabetic neuropathy, and a tiny percentage comes from autoimmune disorders like scleroderma, much of it is idiopathic. That sounds crazy until you realize that, as my favorite hospitalist Dr. Cheng explained to me, much of medicine is idiopathic. We don’t know what causes most cancer or heart disease, for example, even if scientists have identified some risk factors.
Through all of last week (and all of my stay, really), plans and ideas continually changed. Some of you undoubtedly saw my Facebook updates to that effect. Originally, there was some talk of my receiving a J-tube (surgical feeding tube into the small bowel) and a Gastric Electrical Stimulator (pacemaker for the stomach) in the same surgery within a few days. Then, there was talk of a temporary stimulator to do a trial since we didn’t know that the stimulator would work in my case, since my motility is so weird. Then, in part because the holidays were coming up, my doctors decided to wait to do the temporary stimulator until after the first and to have a surgical J-tube placed last week. While in my small bowel, the idea was to take a full muscle biopsy (which is only possible during surgery) to check for some weird muscular diseases since I’ve had other neuromuscular symptoms. I talked to the surgical resident who would be on the surgery with one of the minimally invasive surgeons Tuesday night and she said that the surgery would probably be Thursday or Friday since I wasn’t on the schedule for Wednesday. Then she came back later that evening and said that I was going to have surgery on Wednesday and it would be some time after 2:30. Then she came in early Wednesday morning and said that actually it would be sometime that morning. See what I mean by a roller coaster? And that pales in comparison to what’s coming.
Wednesday morning, not long before I was set to head down for surgery, Dr. Cheng came in to tell me that he, Dr. Shetler, and Dr. Snape had been talking and they decided not to have a surgical j-tube placed just yet. The muscle biopsy was too risky for a shot in the dark and any time you operate on the intestines, you run the risk of creating or exacerbating a motility problem. Since they planned for me to come back in just a couple weeks for a stimulator trial, and nobody could say if I would need a feeding tube long term. And everyone thinks that it’s basically a miracle that I haven’t had abdominal surgery at this point and nobody really wants to be the first one to mess that up.
So this happened:
You may not quite see, but I’m smiling and giving a thumbs up in the second picture. (Thumbs up rock! They basically kept me going through the stay!) I had yet another nasal tube placed at bedside, before being sent down to interventional radiology to have it advanced into my jejunum. Dr. Shetler (my main GI) came by to talk to us about the new plan right as transport arrived to take me down to IR. She said she’d come back but she talked to my parents for a few minutes as I was being wheeled away. The last thing I heard her say as I was being wheeled away was that we were running out of options and if the stimulator didn’t work, we’d be out.
Not. An. Option.
I got down to IR and the nurse assisting the radiologist was the same one I’d had for both my last NJ placement at CPMC and for my Upper GI. She remembered my problems with latex! 😀 I figured out that I was particularly memorable because I was basically the youngest one in the hospital (it only takes patients over 18 and 19 year olds are a notoriously healthy bunch…and still handled through children’s hospitals in a lot of cases.) Also, the tubes help.
The radiologist came in and got to work. He had no trouble advancing it through the pyloric sphincter, but he started to run into problems in my duodenum, which is the first section of the small bowel. He started asking me some questions about my medical history, which I was able to answer. (The nurse was impressed by how much I remembered — a good memory can really come in handy in these kind of situations!) He told me that the first part of my duodenum was baggy and loose like my stomach and then it suddenly became normal right after the part he was having difficulty getting the tube through. He started injecting contrast, which he did several times, and he asked if I’d had an abdominal CT. When I said that I’d had one the previous week, he sent the nurse to pull it up on the computer. He got the tube into my jejunum, then went to look at it. When he came back, he asked me if I’d ever heard of SMA Syndrome.
“Superior Mesenteric Artery,” I said, “I don’t know a lot about it.” I didn’t. I’d come across a few references previously, and they didn’t make it sound good. There’s no good reason for me to have even remembered what it stood for, but I did.
He showed me the x-rays and explained that when he sees a young, thin girl with failure to thrive and gastroparesis-like symptoms and a baggy duodenum that suddenly gets normal, he has a pretty high suspicion of SMA syndrome. He said they see about two cases a year at CPMC, always with my kind of symptoms and body type. He said that my CT does indeed show the characteristically narrowed angle.
What happens with SMA Syndrome is that the eponymous artery, which crosses over the duodenum, ends up compressing the duodenum to the point of partial or even full obstruction. Normally, there should be a pad of visceral fat protecting the duodenum, but sometimes that pad disappears. It’s controversial whether it can be a primary issue or whether it has to be secondary. While at first my doctors kicked around the idea of it being primary, nobody seems to be very convinced by that and the general thought is that some kind of motility issue caused weight loss, which caused SMA, which caused further motility issues and weight loss, which made the SMA worse….They keep emphasizing that my case is complicated for a reason!
The radiologist brought in my parents and showed up the abdominal CT and explained some more about SMA Syndrome. He explained that while everyone’s concern with body habit is about people being overweight, being underweight can be even more dangerous. Losing fifteen or twenty pounds from an already thin frame just isn’t good. He showed me some maneuvers to try if I were able to eat to see if they would help allow for the passage of food through the obstruction. My mom asked him if this meant that I would be able to eat normally once the SMA is fixed and he hesitated, before saying that it would probably take some retraining.
When I got back up to my room, my GI came back by. She hadn’t heard from the radiologist yet, but when I mentioned SMA, it was like a light bulb went off. She said that it could explain my symptoms. It even explains how I haven’t thrown up my NJ tube, despite some serious vomiting — the SMA pinned it in place. When she came back after checking the scans, and the hospitalist also reviewed them, we all came up with a plan of attack: try to put on weight with the tube feeding and see if that resolves the SMA. If it does, we’ll see how many of my symptoms remain and treat accordingly (considering the stimulator if we absolutely have to.) If it doesn’t, then the we’ll have to consider some scarier options (really major surgery, basically.) Hopefully, it won’t even begin to come to that. For a lot of people, restoring the visceral fat does the trick, and I very much hope that I’ll be one of them!
(At this point, I should probably say that if you’ve Googled SMA and seen the crazy high mortality rate, that’s only because it goes undiagnosed so much. When it’s diagnosed and treated accurately, there’s not much of a mortality rate.)
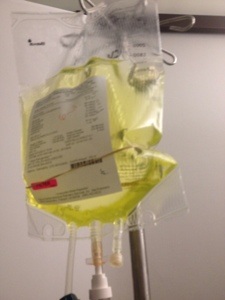
This hasn’t been an easy diagnosis to receive, but we have a plan going forward and something to explain my symptoms and their severity. Over the last few days of my hospital stay, we figured out a formula that I could tolerate through my tube (fourth time’s the charm!) and I’ve been sent home with that and saline/potassium/dextrose infusions through my PICC line. I have a lot of really smart doctors who are thinking things through and each day we get closer to a resolution. I’m stable now and while my situation isn’t entirely tenable in the long term, we have time. My doctors have collected a lot of data and stabilizing me has given them time to go through it and think about it some more.
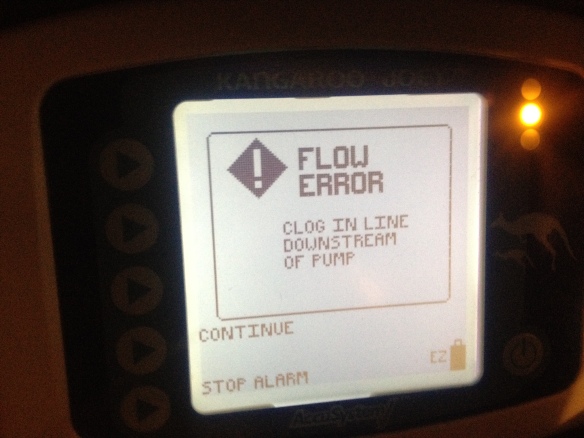
Saturday was a nice and distracting day. I started a better formula, took a shower, had a great visit from my friend Genny who was back in the Bay for the holidays, and got to go through a pole-free walk because my pumps were broken.
 Versus carrying around these kinds of things…
Versus carrying around these kinds of things…
And while I came into the hospital in a wheelchair, I left walking.
I mean it when I say ready for anything. I won’t let a little SMA or gastroparesis get me down!
And a new feature, started at the suggestion of my uncle: foods I’m currently craving! Chocolate (expect to see that always), chocolate fudge, French toast, Atlantic salmon, garlic bread, roasted carrots, ice water.